
We’ve been hearing that a cure for spinal cord injury is just around the corner–five to 10 years in the future–for the past 30 years at least. But what most of us think of as cure–tap dancing, mountain climbing, full restoration to whatever we could do pre-injury–remains an unrealized dream and as illusive as ever. The good news is that numerous procedures and treatments intended to achieve incremental improvements–and with them, significant enhancement and expansion of quality of life–are cropping up all over the globe. We are entering the era of partial restoration.
As always, the bulk of research money and energy is being directed toward finding a cure that will interdict permanent damage during the acute SCI phase. In Florida, Dr. Barth Green of The Miami Project is testing a combination lab therapy on rats that he says he’d put his money on “for sure.” At Purdue University, researchers are injecting spinal cord injured dogs with a liquid polymer that has half of them standing or walking in less than a month. And a U.S. firm, Proneuron, with an Israel-based subsidiary, is offering a surgical technique to people with new injuries both abroad and in the United States. All are procedures that must be performed within two weeks of injury. But other procedures and therapies are being studied and developed around the world that show promise for sub-acute and chronic injuries. Most of them involve helping the body heal itself with its own tissue taken from locations as unlikely as skin, blood, nose or umbilical cord.
One of the most promising treatments for the acute stage is macrophage therapy, popularized a few years ago by the partial success of Melissa Holley, who underwent the procedure in Israel. Justin Richardson, who sustained a C6-7 cervical injury on Aug. 10, 2003, in a diving accident, decided to follow in Holley’s tracks. Within 10 days of being injured, he was headed to the Sheba Medical Center in Tel Hashomer, Israel, just outside of Tel Aviv, for experimental surgery as part of a clinical trial (see sidebar).
Proneuron Biotechnologies’ ProCord procedure takes blood cells called macrophages–a type of white blood cells that play a beneficial role in wound healing and tissue regeneration–and incubates them with skin, during which time they adopt specific properties that support nerve cell survival and repair. These cultured cells are then injected directly into the spinal cord at the site of injury, where they facilitate healing and repair and help the remaining nerves to regenerate following SCI or neurological diseases such as Lou Gehrig’s or Parkinson’s.
Macrophages exist everywhere in the body–lungs, liver, blood, peripheral and central nervous systems. Following tissue injury, macrophages remove cell debris and secrete growth factors which promote inflammation and begin healing. A process called “immune privilege” normally represses this type of healing in the CNS, but in the early 1990s Michal Schwartz, Ph.D., of the Weizmann Institute of Science in Rehovot, Israel, found that specially treated macrophages can actually promote nerve regeneration and the natural activity of the immune system, protecting nerve cells against degeneration and helping in the recovery process. The treatment is used for survivors with complete injuries who undergo the procedure within two weeks of injury, before immune privilege does permanent damage and while the immune system is still responsive to this type of therapy.
“ProCord appears to markedly improve the degree of neurological recovery,” said Dr. Eti Yoles, who directed the research. He adds that in rat experiments the treatment preserved the structure of the spinal cord better, with less cyst formation–a complication normally associated with increased neurological loss and pain.
The present Phase II clinical trial calls for 61 people with acute, complete spinal cord injuries (C5-T11), to be treated within two weeks of injury. Two-thirds of them will undergo the procedure with the remaining third followed as a control group. All participants will receive standard rehabilitation and follow-up testing for one year. Of the 16 people who are at least one year post-procedure, four have progressed to an “incomplete” status; the other 12 remain unchanged.
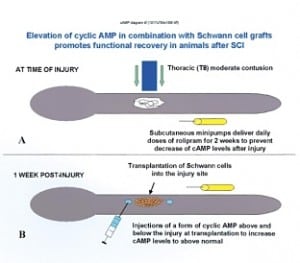
Miami Project: Pearse-Bunge Combination Therapy
Meanwhile, The Miami Project to Cure Paralysis has generated excitement within the SCI research community by promoting healing and regeneration in rats by pairing a specific cell messenger molecule and another substance to counteract and neutralize the hostile, inflammatory response and lower the inhibitory environment that follows injury. Once that’s done, Schwann cells are used to form a bridge across the lesion. These messenger molecules, called cyclic AMP, are found within or around cells and help regulate their workings, activate receptors and send signals telling the cells where and how long to grow. The substance rolipram helps maintain levels of cyclic AMP and decrease the rate at which it is broken down. Together, the two appear to enhance axon survival and may even encourage nerve regeneration. The Schwann cells, which secrete both growth factors and myelin, are then introduced to promote regeneration across the lesion.
Recent published reports show that treated rats experienced a 70 percent improvement in normal walking function, though they still had problems positioning their feet while walking, difficulty with complex movements–such as crossing a horizontal ladder apparatus–and walked with their feet further apart than normal, indicating decreased postural stability. The treatment has only been tried within a week or so of injury, so don’t throw your chair away just yet.
Because rolipram by itself was found to protect the spinal cord from damage and facilitate some improvement in function, the Project is currently determining the best dosing, route of administration and therapeutic window in animals. Miami is also investigating Schwann cell grafts alone and in “triple combination” to promote nerve fiber regeneration, though there is concern that abnormal sensory nerve regrowth might cause or increase neuropathic pain.
“We need to address pain before taking any regenerative therapy to clinical trials,” Maria Amador, the project’s education director says. “We want to increase motor function, but not decrease quality of life by inducing or increasing pain.”
Amador sees this cyclic-AMP/rolipram/Schwann cell therapy as yet another piece of a larger restoration puzzle rather than the silver bullet cure. All three elements have been safely used with humans, so quick FDA approval shouldn’t be a problem, but that’s only the first and easiest step in taking the full therapy forward. The project is also looking at new drugs similar to rolipram, but with fewer side effects.
Simultaneous studies are underway to satisfy human Schwann cell purity requirements and to determine the therapy’s effectiveness with chronic injuries. Until those questions are answered, there are no concrete plans for clinical trials with humans. Still, Miami Project’s Marc Buoniconti says this all holds promise and lays the foundation work for treating chronic injuries.
“This is a giant step in answering the regeneration question,” says Buoniconti, a C4 quad of nearly two decades. “Rolipram and cyclic AMP break down the communication barriers between cells so they can communicate with each other and begin to regenerate. The theory goes that with a chronic injury, if we cut out the lesion and a miniscule amount of viable tissue at each end, we essentially create a new injury, which allows us to then apply the ‘triple combo therapy.’ For now, the operative word is ‘theory.'”
Polyethylene Glycol: Repair Agents
In December 2004 researchers at Purdue University reported that a liquid polymer known as polyethylene glycol (PEG), if injected within 72 hours of serious spinal injury, can prevent permanent spinal damage in recently injured dogs. The treatment prevents nerve cells from rupturing beyond repair and helps them heal themselves so they can continue to carry nerve impulses from one cell to the next. It prevents poisonous chemicals from seeping out and doing more damage than the initial injury–resulting in irreparable damage and partial or complete paralysis. The treatment remains experimental and only for animals. A division of Medtronic, a medical technology firm, has secured the commercial rights to the technology.

“In most dogs, we found a PEG injection within 36 hours restored some sensitivity and even mobility within three weeks,” said Purdue’s Center for Paralysis Research director, biophysicist Richard Borgens. “Nearly 75 percent of the dogs we treated were able to resume a normal life; some went on as though nothing had happened. More than half were standing or walking within two weeks of treatment,” Borgens said. “We often saw positive signs within three to five days.”
Borgens spoke of the advantages of using dogs. Unlike rodents, canines don’t experience occasional spontaneous recovery of function following injury. And because all the dogs in this study were injured accidentally, they weren’t under anesthesia at the time of injury, which can act as a protective factor.
“The dirty little secret of rodent work,” Borgens says, “is that they walk after SCI; dogs sort of, man never.”
One big challenge: some control of walking in dogs actually takes place in the spine; in humans it’s all in the brain.
Of the 19 paraplegic dogs treated, seven of them recovered measurable proprioception, 13 were ambulating within six weeks of treatment and only three remained completely paraplegic. Seven of 11 demonstrated regained nerve transmission across the lesion. Thirteen of the 19 dog owners later reported their pets had regained continence. Three or four recovered so completely as to appear “normal” to the untrained observer. Improvement criteria included ability to move, deep and superficial pain perception, and transmission of electrical impulses across the lesion site. There were no reported side effects. The next step is human trials, possibly within 18 months.
“But we don’t anticipate this to have any effect on people with chronic injuries,” Borgens says. “We hope PEG will prevent permanent paralysis in new injuries and would like to see it in every ambulance.”
Researchers at Purdue are also attempting to regenerate injured spinal cord nerve fibers by implanting a small device called an extraspinal oscillating field stimulator, which produces a weak electrical field across the injury site for approximately 14 weeks. The units, about twice the size of a lipstick case, were tried on dozens of dogs, then in a limited study of 10 people and now with 10 more people. The treatment must be done within 18 days of injury, so again oldtimers with chronic injuries are on hold. Electrical fields are a normal part of wound healing and embryonic development, particularly the nervous system.
Modest improvements in American Spinal Injury Association muscle and sensation scores, as well as measurements of electrical impulse transmission across the lesion site fell in the “statistically significant” range. One of the 10 participants recovered enough sexual sensation to achieve a pleasurable orgasm. Two recovered some lower-extremity function. No one reported increased pain perception or any other ill effects.
Promise for Sub-Acute and Chronic Injuries
Macrophage, Schwann cells and stem cells may get all the publicity, but that doesn’t mean they’re the quickest route to the cure. And it doesn’t mean that cure will be developed in this country. Scientists and surgeons are working tirelessly around the world in search of answers. Most agree that the body’s own tissue holds the keys to enhanced physical function and improved quality of life.
One approach has shown significant promise and tangible results for those with injuries in the sub-acute phase–at this point up to nine years post-injury. Olfactory tissue harvested from nasal passages contains many different types of cells with regenerative potential, including renewable neurons, progenitor stem cells, and remyelinating olfactory ensheathing cells (OEC) that promote regrowth of axons. Animal studies in Madrid, London, Yale University, Australia and Birmingham, Ala., all offer results ranging from regrowth and remyelination of axons to functional improvements such as weight-bearing, locomotion and sensory perception.
Dr. Carlos Lima of Lisbon, Portugal, has taken the OEC procedure into the human arena. As of this writing, he has done the procedure on 43 people from a number of countries. While it’s still early to discuss results–the restoration process can go on for at least a few years–many have reported increased abdominal muscle control, regained grasping ability, gluteus and leg abductor control, bladder control and improved sensation. In Australia, eight patients have received a similar treatment as part of a Phase I risk/benefit trial. No results have been reported.
Several Americans have traveled to Portugal to undergo the OEC procedure as part of a collaborative program headed by Dr. Steven Hinderer at the Rehabilitation Institute of Michigan. After surgery, the participants return to RIM for intensive physical therapy, which Hinderer considers critical for optimum recovery. [For an up-close look at Hinderer’s collaborative international program, see “SCI Recovery: The Nose Knows,” page 41.]
Another approach that holds promise for those with older injuries is called peripheral nerve rerouting. This procedure is essentially a nerve bypass using peripheral nerves emanating from the spinal cord above the site of injury, rerouting and connecting them to nerves below the level of injury. This bridging of the interrupted circuit of the central nervous system re-establishes a functional connection from the brain to muscle and sensory systems below the site of injury. Surgeons in China and Italy are using this procedure in an attempt to selectively restore respiratory, bowel, bladder, sensation and muscle function.
In one variation of the rerouting surgery, both a section of peripheral nerve and the spinal cord are scraped to expose nerve fibers, glial cells and other beneficial factors. The two are then placed in direct contact with each other. The grafts contain Schwann cells, fibroblasts and trophic factors, which promote axonal regeneration and restore some connection through the injury site.
Dr. Shaocheng Zhang of Shanghai, China has performed over 100 such procedures both in China and, at the request of its president, in Iceland. In one study of 35 incomplete injuries, 32 experienced some increased upper leg muscle strength and ambulatory ability. In another, 26 of 30 experienced substantially better bowel and bladder sensation, function and control. In a third, 18 of 23 paras with complete injuries regained enough lower body function to walk, on average, over 600 yards using crutches or walkers. This group had T8-T12 injuries of less than three years duration, spastic paralysis, and muscle tone sufficient to bear weight prior to surgery.
To the press and general public, walking has always been associated with SCI cure, and the presumptive frontrunner, at least in theory, is considered by many to be stem cells. This past November Hwang Mi-Soon of South Korea, paralyzed two decades ago at 17, stood up and took a few steps wearing long leg braces and using a walker only three weeks after surgery. Mi-Soon reported sensory and motor improvement and was moving her hips within 15 days of the procedure and said her feet responded to stimulation in about a month.
Hwang was paraplegic but no level of injury was reported in available published reports. Scientists in Seoul claim to have repaired her damaged spine by injecting stem cells isolated and cultured from umbilical cord blood at the site of the lesion. These “multipotent” stem cells found in cord blood are more limited than embryonic stem cells in the number of specialized cell types they can form. But unlike embryonic stem cells, they don’t tend to form tumors or trigger much of an immune response. This would be the world’s first case of a successful umbilical cord blood stem cell treatment for SCI and could emerge as an ethical and safe alternative to embryonic stem cells. However, the government-supported research still needs to overcome difficulties in isolating the stem cells from the blood, making donor-recipient genetic matches and refining the exact location for cell transplantation. Nothing related to the procedure has appeared in any professionally recognized publication.
Published reports stated that Mi-Soon had been bedridden since her injury nearly two decades earlier, a suspiciously odd circumstance for a para. Moreover, many researchers claim that the reported recovery occurred much too quickly to be attributed to axonal regeneration and stem cells doing their thing. One plausible explanation is that chemicals secreted by the injected cells improved the environment in the spinal cord, thereby enhancing the function of some of the surviving spinal cord nerve cells. This is similar to the outcomes of olfactory ensheathing cell injections done in Beijing and Australia.
Embryonic Stem Cells and the Future
For all the talk, promise and hope, two decades of embryonic stem cell research have yet to yield a single human clinical trial. Brad Duerstock, Ph.D., a neurobiologist at the Purdue lab and himself a C4-5 quad since 1989, seems skeptical that cell replacement can live up to the promise.
“I’m a big advocate for Parkinson’s and other diseases, but with SCI, we’re losing cell fibers that begin maybe in the brain stem and run all the way down the cord. We’re expecting a lot of them to grow and reconnect properly. There’s a lot of work to do.”
Still, with recent commitments by the states of New Jersey and California, it appears that embryonic stem cell research will pick up steam in the years to come. Look for New Mobility to cover the latest on “The Stem Cell Challenge” in an upcoming issue this fall.
In the past decade we’ve seen at least 10 Phase I trials in acute and chronic SCI using a variety of procedures, drug therapies and physical modalities. They’ve all made splashes, big and small–but we’re still sitting.
For years methylprednisolone was routinely given following injury, until side effects made it optional. Frampadine (4-AP) showed great promise in mitigating the effects of chronic injuries but then was pulled. Neurotrophic factors come with huge side effects. Christopher Reeve and Dr. John McDonald’s work with functional electrical stimulation and gravity-assisted walking have shown promise, but insurance companies are slow to cover it. In the early 1990s omentum wraps made a big splash, but hardly a ripple now. If you’re paying attention, patience is indeed a virtue.
Unless you’re willing to travel the globe for somewhat exotic and unconventional procedures scoffed at by the American Medical Association, complete “cure” remains an elusive concept. And as long as there is denial of the complexity and severity of SCI, there will be those offering hype and miracles. Does this mean it’s time to throw in the towel? Of course not. Recent advances in restoration, although partial, are undeniable. Sam Maddox, founder of New Mobility and now Knowledge Manager for the Christopher and Dana Reeve Paralysis Resource Center, is in touch with leading SCI researchers. “According to the scientists,” says Maddox, “the last year or two have been more fruitful than the previous 10.”
Each small clinical success provides more answers to basic regeneration and cure questions. Many scientists believe that finding effective treatments–or even that breakthrough “cure” procedure–will require combination strategies to restart nerve fiber growth and influence where fibers grow and how they make connections. Each new answer offers hope, if not for outright cure, then certainly for partial restoration–and we all know how small improvements in function translate into big changes in quality of life.
“There’s always hope,” says Duerstock. “This could be like polio where we dramatically decrease the number of new injuries. The pathologies of acute and chronic injuries are totally different. The acute ones are easier to treat and what we learn with them will help us with chronic injuries.”
In the meantime, don’t forget to have fun. Life is what happens while you’re waiting for the cure.
Justin Richardson, C6-7, ProCord Pioneer
 I have absolutely no regrets about the procedure or the study that followed it and would strongly encourage anyone contemplating the procedure to give it serious consideration. I feel it’s changed my life for the better in more ways that I could ever begin to put into words.
I have absolutely no regrets about the procedure or the study that followed it and would strongly encourage anyone contemplating the procedure to give it serious consideration. I feel it’s changed my life for the better in more ways that I could ever begin to put into words.
Recovery and regeneration have progressed very slowly but steadily since surgery. I began to notice return of light touch sensation within three weeks of surgery, though it began very spottily and wasn’t consistent. Over time, the sensation returned to much of my upper body and is now “normal” to the T6 level. After about nine months, I regained bladder sensation, allowing me to catheterize on an as-needed basis rather than on a schedule and that gave me more confidence and freedom in social situations. Within a year, all the muscles in my hands and arms had returned to functional status and are almost 100 percent normal. I can’t think of anything I can’t do with my hands now that I could not do before my injury. I cook, clean, drive, take notes, and I do it all without help.
I will finish my degree at North Carolina State University, taking only one extra semester, and then I’ll start working. My social and dating lives have not slowed in the slightest; if anything, they’ve both picked up. I haven’t regained any functional use of my legs or lower extremities and still use a wheelchair. I would classify myself as a high or mid para. However, I now take 100 percent care of myself and feel confident that one day I’ll be able to take care of others. I can’t wait to begin my own family.
For a complete list of Proneuron (ProCord) treatment protocol/follow-up sites and clinical teams, visit www.spinalcordtrial.com or e-mail clinical.trial@proneuron.com. For inquiries, call 866/539-0767 or 506/652-3486.
Miami Project Combination Therapy at a Glance
- Injured animals improved to 70 percent of normal walking function, demonstrating better coordination, foot placement and stability.
- The treatment saved axons from dying and resulted in more axons within the Schwann cell grafts.
- Axons from neurons in the brain grew their fibers not only into but also beyond the grafts and into the spinal cord.
- The initial rolipram treatment prevented the decrease of cyclical-AMP in the central nervous system after injury and the later treatment increased levels to above normal, important for growth of axons across inhibitory environments.
Support New MobilityWait! Before you wander off to other parts of the internet, please consider supporting New Mobility. For more than three decades, New Mobility has published groundbreaking content for active wheelchair users. We share practical advice from wheelchair users across the country, review life-changing technology and demand equity in healthcare, travel and all facets of life. But none of this is cheap, easy or profitable. Your support helps us give wheelchair users the resources to build a fulfilling life. |


Recent Comments
Bill on LapStacker Relaunches Wheelchair Carrying System
Phillip Gossett on Functional Fitness: How To Make Your Transfers Easier
Kevin Hoy on TiLite Releases Its First Carbon Fiber Wheelchair