Loss of Function Years after SCI:
When to Have Untethering Surgery
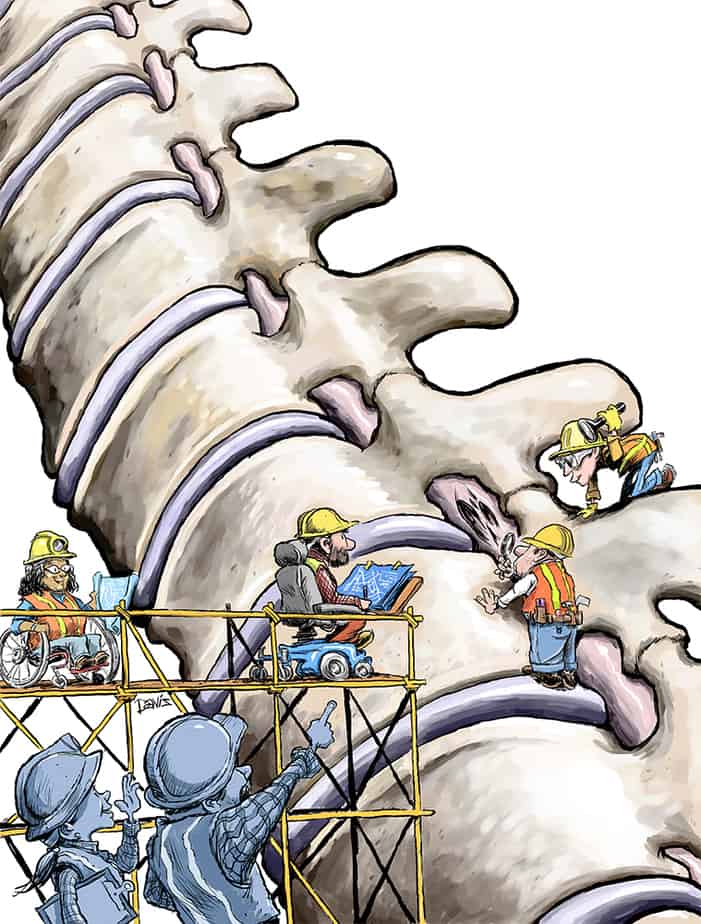
Following spinal cord injury, most of us who are paralyzed think in terms of what has been lost below the level of injury. But what is more worrisome is the possibility that damage can also go the other way, ascending to higher levels in the cord, resulting in possible additional motor and sensory loss, increased spasticity, pain and more. Worse yet, it can happen years after the initial injury.
Also see:
|
Brook McCall is weighing her options. She is worried. Seventeen years ago when she left Craig Hospital with a C4 SCI from a fall, she had been told, almost as an afterthought, that she had a small, bubble-sized cyst just above her C4 damaged cord, and that it would be a good idea to keep an eye on it, as if that is even possible. Odds are it would not be a problem, they said, but scar tissue from the injured cord can cause tethering, sometimes giving rise to a cyst, also called a syrinx, which can trap cerebrospinal fluid and expand, sometimes climbing higher in the spinal cord. While tethering, also called adhesions, in various degrees occurs in virtual all SCIs, when a cyst forms and traps CSF, it’s called syringomyelia, which affects an estimated 10% to 20% of SCI survivors. Serious complications can follow.

Eight years later, McCall noticed that one of her eyelids began drooping intermittently. Was this a sign of Horner’s syndrome, a symptom of syringomyelia she had been warned to watch for? A drooping eyelid may seem like an unlikely symptom related to spinal cord injury or disease, but it is a symptom nonetheless.
“I went to a neuro-ophthalmologist in San Diego,” she says. “He said it was ptosis, the medical term for drooping eyelid, and nothing to worry about. I wanted to believe him, but as the drooping came and went, I knew it wasn’t normal. I mentioned Horner’s syndrome and my cyst to every new physician I encountered, but it was always casually brushed off. I stopped asking after one blankly said, ‘Horner’s syndrome! That’s really serious, you don’t want that.’ He was right, but I tried to let it go.”
Four years passed with no changes, but the thought of Horner’s syndrome stuck in her mind anytime she felt pressure on her eyelid. Not long after that she went back to Craig Hospital for a reevaluation. “I requested an MRI, but they didn’t think it was needed. That year I went from having little to no pain to having severe low and mid-back pain with intense spasms and stiffness. I went to Oregon Health Sciences University and got opinions from two different neurosurgeons.”
She had two MRIs and a CT scan. “The first neurologist told me it would not be worth it to work on me because he wasn’t concerned about what I had to lose because of my limited function as a high quad. I told him, ‘How dare you say that? I have a lot to lose.’ But he really didn’t care.”
The second neurosurgeon was more compassionate. “He said it looks like I needed to have untethering surgery and drain the syrinx in order to preserve what function I had. If I ignored it, symptoms other than Horner’s syndrome could possibly come into play — further loss of motor and sensory control, more pain, more stiffness and spasticity.” The syrinx had moved and expanded, and McCall had seen the MRI films. “It was upsetting to look at,” she says. “The cyst was small at first, but it had moved up a full vertebra, then narrowed and went all the way to my brainstem. It was a hard conversation to have.”
After a good deal of consideration, she decided to go back to Craig Hospital, have another evaluation and see Dr. Scott Falci, a respected neurosurgeon with well over 1,000 untethering/syrinx surgeries. His initial assessment was that she is not in immediate danger, but she is still uncertain about how she will proceed. In recent months, the stiffness, pain and spasticity have increased dramatically, and the thought of a fluid-filled cyst expanding near her brainstem is a constant worry. Although Falci can’t predict what the specific outcome of surgery may be, he claims to have a 90% success rate at stopping further expansion of the cyst, at least.
Loss of Strength: A Major Symptom
Kent Petersen rehabbed at Craig Hospital but didn’t see or hear of Falci during his initial stay. At the age of 58, he injured his spinal cord at the T7 level in a serious skiing accident that also broke ribs, punctured a lung and fractured his neck. “I was an all-out skier, hauling ass when it happened,” he says. Fortunately, there was no damage to his spinal cord from the neck injury.
Almost two years passed before he started noticing he was losing strength in his left arm and hand. “It was a gradual loss over a few months, but when it got to where I couldn’t write, I contacted Craig Hospital and went in for an evaluation. I had no idea what it was. It was a scary proposition.”
They did an MRI on his torso, neck and head. That’s when he met Falci. “He said it was a problem with adhesion — scar tissue adhering to the dura,” the outermost covering of the cord. In other words, he had a tethered cord. Petersen had never heard of it. It turned out there was also a small cyst above T7 that needed a self-dissolving shunt to drain.
“I was kind of complacent about the surgery, probably because I’d had a number of surgeries,” he says. “I thought I could handle it without a problem. I tell you, the surgery kicked my ass. I woke up in a lot of pain and extreme disorientation. I think the drugs were still affecting my state of mind. The nurse told me the next day, laughing, ‘you were pretty certain you were going to die.’”
Today, two years following his untethering surgery, he’s glad he went through with it. “Smart thing I took care of this,” he says. “I totally trust the people at Craig.”
Prior to the surgery he also had pain in his left arm and hand. There has been little change in pain since then, but he’s OK with it. “The good news is I have recovered the strength I lost. In fact, I’m stronger now than I’ve ever been since the accident. The main thing I was afraid of was loss of function. From that standpoint, the operation was a complete success.”
Loss of Sensation
While snow sledding in 2005, Dave Denniston, an NCAA champion swimmer who just missed out on the 2004 U. S. Olympic team, hit a tree and sustained a T10-11 SCI. Two years later he started having pain and numbness. “It started in late 2006, pain when I sneezed or coughed. A sharp pain followed by momentary numbness. Seemed like every time I did this, I felt the pain go a little higher on my left side.” At the time, he had made the transition to Paralympic swimming and was in training for the 2008 games in Beijing, so his main concern was that motor loss might follow the pain and loss of sensation.

“I went to a neurosurgeon. He thought it might be cancer in my cord and wanted to take a biopsy from my neck. I said I’ll pass and began looking for a second opinion.” He found Dr. Ulrich Batzdorf at UCLA, a well-known neurosurgeon, who diagnosed it as syringomyelia.
Batzdorf supervised the surgery in August of 2007. “They did some untethering, drained the cyst and reinforced the cord with GORE-TEX sheathing for protection. Whatever they did, it must not have been enough. Also, I might have pulled a bonehead stunt by pushing myself more than I should have when I returned to training. Too much exertion might have been a factor.” In late 2007 symptoms returned — pain and numbness on his left side. Fluid was still finding a way to get trapped in the center of the cord.
“I was afraid I might lose all sensation on my left side and end up like a stroke victim, so I went to Dr. Scott Falci at Craig. He said the cyst had moved from T10 all the way up to C4. It was frightening. I saw the images myself,” says Denniston. “It went all that way and was about the diameter of a pencil before it was drained and released.”
In April 2008, Falci did a second untethering surgery and inserted a shunt to keep the CSF flowing. “After the surgery I was in a lot of pain, a kind of radiating ache in my body. It maybe lasted about a week.” After the pain subsided, Denniston was able to return to training, and over the next two months Falci did two follow-ups and another MRI. “It all looked OK. I had some muscle tightness in my back but worked it out with massage and exercise.”
It took about four months for Denniston to recover. He competed in the Beijing Paralympic Games in September 2008. “Now I’m great, pretty much normal, lost just a little bit of sensation on my left side. I have to be careful when I grab stuff with my left hand out of the microwave, that kind of thing. But no usage problems. I lost a little in my stabilizer muscles on my left side, so it affects my posture and stability in a minor way. What I feel most is fatigue there sooner than other places. No one would ever notice it, just something that I feel. I’ve been pain-free for more than a decade now.”
Now Denniston is head coach of the men’s swim team at the University of Wyoming. He and his wife live in Laramie, Wyoming, not far from the site of his sledding accident. He has learned to stress the importance of recovery time for his swimmers. “Allow time to let your body recover. I preach that a lot.” He still swims regularly.
Breathing Problems and Pain
A year after Ali Ingersoll sustained a C6 SCI from a shallow diving accident in the Bahamas, an MRI showed a syrinx near the injury in her spinal cord. If the fluid-filled syrinx moved higher, say to C4, it could result in breathing problems. If that happened, would she ever be able to regain what she was likely to lose?
Concerned about losing function, she spoke with multiple surgeons, including the Miami Project’s Dr. Barth Green, a leading expert, but didn’t find any who thought she was in immediate danger. Because of the high risk of the surgery, no one wanted to surgically intervene.
Ingersoll and her family disagreed and began searching for alternatives. Her father, with a background in science and ever the diligent detective, met Dr. Wise Young of Rutgers University, a global leader in the field, who facilitated a trip to China to observe a spinal surgery. The neurosurgeon was Dr. Lansheng Liu, who Young enthusiastically endorsed.
Ingersoll and her family moved to China to begin planning the removal of her syrinx at Tongren Hospital in Kunming, where Liu was the lead neurosurgeon. As an added benefit, Tongren Hospital was one of the sites conducting an experimental locomotor-based walking program, and Ingersoll would be able to participate after her surgery. Ingersoll also hoped the surgery would relieve her moderate to severe neuropathic pain.

When they got settled in Kunming, her symptoms got worse. “Within about two or three weeks of our arrival, I was on oxygen for most of the day and afraid it could get worse,” says Ingersoll.
The surgical team, led by Liu, had to perform a triple laminectomy just to gain access to the problem area. It isn’t unusual for untethering/syrinx surgeries to take up to 10 or 12 hours, but the highly experienced Chinese team completed the operation in less than half that time.
After recovering from her surgery, she began the walking program, but on the first day of standing in a walker, aided by helpers, she experienced severe autonomic dysreflexia. Tests discovered fractures in her femur and tibia — her walking program was over before it got started.
The good news is she is happy with the results of the untethering surgery, calling it “a net-net success.” No more breathing problems. On the pain front, however, more disappointment. “No change in neuropathic pain,” she says, “plus I ended up with persistent chronic pain in my neck.” (For more on Ingersoll’s experience, see her story To China and Back for Syrinx Surgery.)
* * *
McCall, Petersen, Denniston and Ingersoll each had different symptoms — a drooping eyelid, stiffness in the back and neck, increase in spasticity, loss of strength, loss of sensation, breathing problems and pain — which can diminish, linger or sometimes increase following surgery. Their combined stories serve as an example of how confronting worrisome symptoms, rather than downplaying or ignoring them, is a smart course of action. No one wants to lose more function than they lost at the time of injury.
Since we are entering a time of greater understanding of how the spinal cord can regenerate and damage can be reversed, syringomyelia may soon be a problem of the past. And there is even more reason for hope. Recent research has shown that untethering — when no syrinx has formed — may actually help restore some functions that were lost at the time of injury.
Opening Up New Possibilities
When untethering was included in clinical trials at Tongren Hospital in Kunming, China, where Ali Ingersoll had her surgery, surprising results occurred. The trials, organized by Young (results published in 2016), combined implantation of umbilical cord blood mononuclear cells followed by intensive locomotor training. This resulted in return of limited walking function for some. Surprisingly, some participants also regained bladder and bowel function. Moreover, a sub-group that included untethering surgery showed an even greater percentage of participants who regained bowel and bladder function.
A more recent follow-up trial in Kunming, as-yet unpublished, focused on untethering surgery and locomotor training with no cell implantation. The official data for this latest study is not yet available, but Young has told NEW MOBILITY that 80% of the untethered subjects regained bladder and bowel function, and many of them now no longer use catheters. “Bowel and bladder recovery appear to be a result of locomotor training increasing the excitability of the lumbosacral spinal cord,” says Young. “Untethering surgery appears to help increase the incidence of bowel and bladder recovery. This is, to my knowledge, the first study to show that untethering surgery will restore bowel and bladder function if it is accompanied by intensive locomotor training. The untethering surgery is actually more than just removing adhesions. All causes of compression and adhesions were removed. The goal of the surgery was to restore pulsatile cerebrospinal fluid flow in the spinal cord.”
Up to this point, Young’s research has concentrated on umbilical cord blood mononuclear cells. It is notable that Young is no longer characterizing cell transplantation as necessary to recover function. He has now become an advocate for intensive locomotor training — six hours a day, six days a week, for six months. He refers to this as the 6-6-6 program.
From a practical perspective, however, intensive LT requires a substantial investment of time, energy and total commitment, as well as funding. Outside of clinical studies and their limited number of participants, programs that offer this are not widely available. And those private programs that are open to the paying public would cost a great deal of money and time as well. Many SCI survivors have jobs, families and other commitments. Clearly, as promising as it may be, intensive LT, at least at this time, will work for only a relatively small percentage of chronic SCI survivors.
Young knows this, and he is doing his best to get trials going in the United States as well as China and India. He is also planning U.S. trials for quads involving restoration of arm and hand function based on the principle of LT, in 2020.
Support New MobilityWait! Before you wander off to other parts of the internet, please consider supporting New Mobility. For more than three decades, New Mobility has published groundbreaking content for active wheelchair users. We share practical advice from wheelchair users across the country, review life-changing technology and demand equity in healthcare, travel and all facets of life. But none of this is cheap, easy or profitable. Your support helps us give wheelchair users the resources to build a fulfilling life. |


Recent Comments
Bill on LapStacker Relaunches Wheelchair Carrying System
Phillip Gossett on Functional Fitness: How To Make Your Transfers Easier
Kevin Hoy on TiLite Releases Its First Carbon Fiber Wheelchair